Saliva Protects Teeth. Dry Mouth Dramatically Raises Decay Risk.
Dry mouth isn’t just uncomfortable — it’s a biological risk factor.
Most people think cavities are caused by sugar.
Sugar matters, but it’s not the full story. The real driver behind tooth decay is not just what you eat — it’s the environment your teeth live in. And one of the biggest factors controlling that environment is something most people ignore until it becomes a problem: saliva.
Saliva is not just “spit.” It is one of the body’s most advanced protective systems. It cleans, repairs, neutralizes, lubricates, and defends. When saliva is present and healthy, teeth have a fighting chance even with imperfect habits. But when saliva drops — even slightly — decay risk rises fast.
At True Balance Dental, Dr. Daniel Ghorbani sees this all the time in patients from Bothell, Bellevue, Kirkland, Seattle, and Lynnwood. Many people do “everything right” but still develop cavities around old fillings, between teeth, or near the gumline. When that pattern repeats, one of the first questions should be: Is the mouth dry? Because dry mouth quietly changes the entire biology of the mouth.
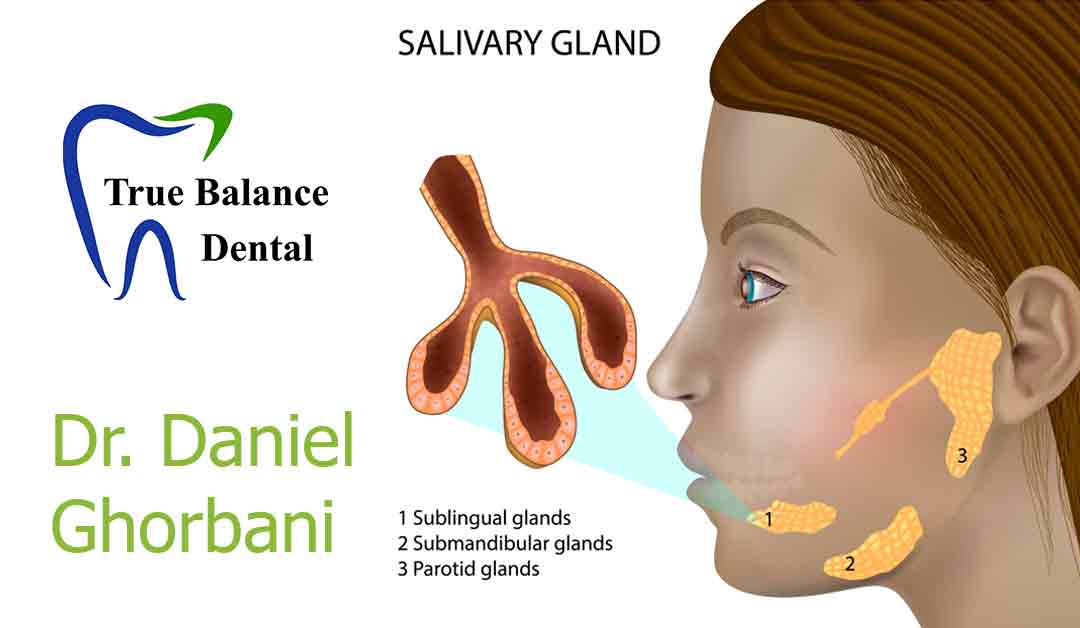
Saliva is your mouth’s natural defense system
To understand why dry mouth is so serious, you have to understand what saliva actually does.
Saliva is a protective fluid made of water, minerals, proteins, enzymes, and immune compounds. It performs several critical functions at the same time.
First, it washes away food particles and reduces bacterial buildup. It doesn’t replace brushing, but it acts like a constant “rinse cycle” that runs all day long.
Second, it neutralizes acid. Every time you eat or drink, bacteria create acids that lower the mouth’s pH. Acid is what damages enamel. Saliva buffers that acidity and pushes the environment back toward neutral.
Third, saliva helps rebuild enamel. Teeth are not dead rocks. Enamel can remineralize in early stages, but only when minerals are available — and those minerals come from saliva.
Fourth, it protects gums and soft tissues by keeping everything lubricated and resilient. Dry tissue is fragile tissue. Dry tissue becomes inflamed easily.
So saliva is not optional. It is the mouth’s built-in immune and repair system.
When saliva drops, decay risk doesn’t rise slowly — it rises sharply
Many people assume a dry mouth is just annoying.
They think it means more thirst, mild discomfort, or maybe bad breath. But biologically, dry mouth is much more important than that. Because when saliva is reduced, the mouth becomes a more acidic, bacteria-friendly environment — and the teeth lose their natural protection.
This creates the exact conditions cavities need.
One reason dry mouth is so dangerous is that it often causes “hidden decay.” Cavities form:
-
between teeth
-
around old fillings or crowns
-
near the gumline
-
under the surface where enamel looks intact
Patients often say, “I don’t understand. I brush. I don’t even eat sugar.” And that can be true. But if saliva is low, the protective system is weakened — and bacteria do what bacteria do.
This is why dentists take dry mouth seriously. It is not a minor symptom; it is a clinical risk factor.
The mouth is an ecosystem, and saliva controls the balance
Your mouth is not sterile. It’s an ecosystem.
The goal is not to kill all bacteria. The goal is balance — healthy bacteria dominating over harmful bacteria.
Saliva is one of the main forces that maintains that balance. It discourages bacterial overgrowth and keeps the oral microbiome stable. But when saliva decreases, harmful bacteria multiply faster. They produce more acid. The mouth becomes more inflamed. Bad breath becomes more persistent. Gum irritation increases. And cavities appear more frequently.
This is where a whole-body perspective becomes essential. Dry mouth is rarely just “a mouth problem.” It often reflects something happening in the bigger system.
Dry mouth is often caused by things outside the mouth
One of the biggest mistakes people make is assuming dry mouth is just dehydration.
Dehydration can contribute, but it’s not the main cause in many cases. Common drivers include medications, stress, mouth breathing, and sleep issues.
In fact, medications are one of the most common causes of dry mouth. Many prescriptions reduce saliva flow as a side effect, including medications for allergies, depression, anxiety, blood pressure, ADHD, and pain management. Patients may take these medications for years without realizing they’re increasing cavity risk.
Stress is another major factor. Stress shifts the nervous system into a sympathetic (“fight or flight”) state, and digestion-related functions — including saliva production — often decrease.
Mouth breathing and sleep-disordered breathing can dry the mouth dramatically. People who sleep with their mouth open may wake up with a dry tongue, sore throat, and bad breath. This is not just a sleep issue — it’s a dental risk factor because the mouth stays dry for hours.
And age plays a role too. As people get older, salivary glands may produce less saliva, especially with medication use and chronic inflammation. That’s one reason dental decay can accelerate later in life even with consistent hygiene.
Saliva protects teeth in a way no product can fully replicate
There are excellent tools available — prescription fluoride, remineralizing agents, xylitol products, saliva substitutes — and they can help. But they do not fully replace natural saliva.
Saliva is dynamic. It adjusts constantly. It changes during eating, speaking, and sleeping. It delivers minerals exactly where the teeth need them. It contains immune compounds that actively manage bacteria.
No mouthwash can match that. No toothpaste can replace that. No dental procedure can permanently compensate for that.
That’s why the focus at True Balance Dental is not just “fix the cavity.” It’s “why did this cavity happen?”
If the patient has dry mouth, the best dentistry is prevention-oriented and system-aware. Otherwise, the cycle repeats: filling after filling, crown after crown, with no real improvement in risk.
Dry mouth doesn’t just affect teeth — it affects gums and infection risk
A dry mouth is also more prone to gum inflammation and infection.
Saliva supports the health of gum tissue by keeping it lubricated and resistant to irritation. When tissues dry out, inflammation becomes easier. Bleeding increases. Gum disease risk rises.
Dry mouth can also increase susceptibility to oral yeast infections and sore spots. Patients sometimes think they have “sensitive gums,” but the real issue is dryness that’s weakening tissue defenses.
Again, the mouth is not separate from the body. When a protective fluid like saliva decreases, the entire environment becomes unstable.
How you know dry mouth is affecting your dental health
Some symptoms are obvious, but many are subtle. Common signs include waking up thirsty, frequent sipping of water, bad breath that returns quickly, sticky saliva, burning tongue, or difficulty swallowing dry foods.
But sometimes the biggest clue is what a dentist sees: repeated cavities in unusual patterns, especially along the gumline or around existing dental work.
Those patterns often tell the truth before symptoms do.
What to do if you have dry mouth
If you suspect dry mouth, the goal is not to simply “drink more water.” Water helps, but it does not fix the biology. The smarter approach is identifying why saliva is low and protecting teeth proactively.
That can include:
-
evaluating medications that reduce saliva
-
addressing mouth breathing and airway issues
-
improving sleep and stress regulation
-
using fluoride and remineralizing strategies when appropriate
-
reducing acidic drinks and frequent snacking
-
focusing on prevention before decay becomes structural damage
The earlier this is addressed, the easier it is to prevent ongoing dental breakdown.
The other half of cavity prevention
Most people are taught that cavity prevention is brushing and flossing.
Those matter. But the other half — the part most people miss — is saliva. Saliva determines whether the mouth is acidic or balanced, whether bacteria dominate or remain controlled, and whether enamel is under attack or able to repair itself.
When saliva is healthy, teeth are protected.
When saliva drops, decay risk climbs quickly.
Dry mouth is not a small detail. It is a shift in the body’s protective system. If you want long-term dental health, you don’t just treat the tooth — you support the environment that protects the tooth.
That is preventive, health-centered dentistry: calm, intentional, and aligned with the whole body.